Technology can help link patients with prediabetes to local lifestyle-change programs, but the bonds between the referring physicians and the community organizations that run the programs cannot be maintained by electronic communication and data-sharing alone.
That was a message delivered this week by Kate Kirley, MD, a family physician and director of chronic disease prevention at the AMA, and Mamta Gakhar, director of health care integration at YMCA of the USA, during the Health Information and Management Systems Society (HIMSS) Global Conference and Exhibition in Orlando, Florida.
The AMA offers tools and resources for physicians and their care teams, as well as online CME to help expand your knowledge in prediabetes and chronic disease treatment.
The relationship between the organizations is more important than the technology, Dr. Kirley said during the presentation, entitled “Bidirectional eReferrals Between Health Systems and YMCAs.”
Some 84 million U.S. adults have prediabetes and 90 percent do not know it, according to the Centers for Disease Control and Prevention (CDC). But structured lifestyle-change programs, such as those offered by the YMCA, can stop the progression of prediabetes to type 2 diabetes. The presenters cited one study that showed how these programs can lower the risk of developing type 2 diabetes by 58 percent, while the glucose-lowering drug metformin only lowered the risk by 31 percent.
The year-long YMCA program includes 25 sessions led by a trained lifestyle coach using a CDC-approved curriculum. The aim is to lower body weight by 5 to 7 percent and to raise physical activity to at least 150 minutes per week.
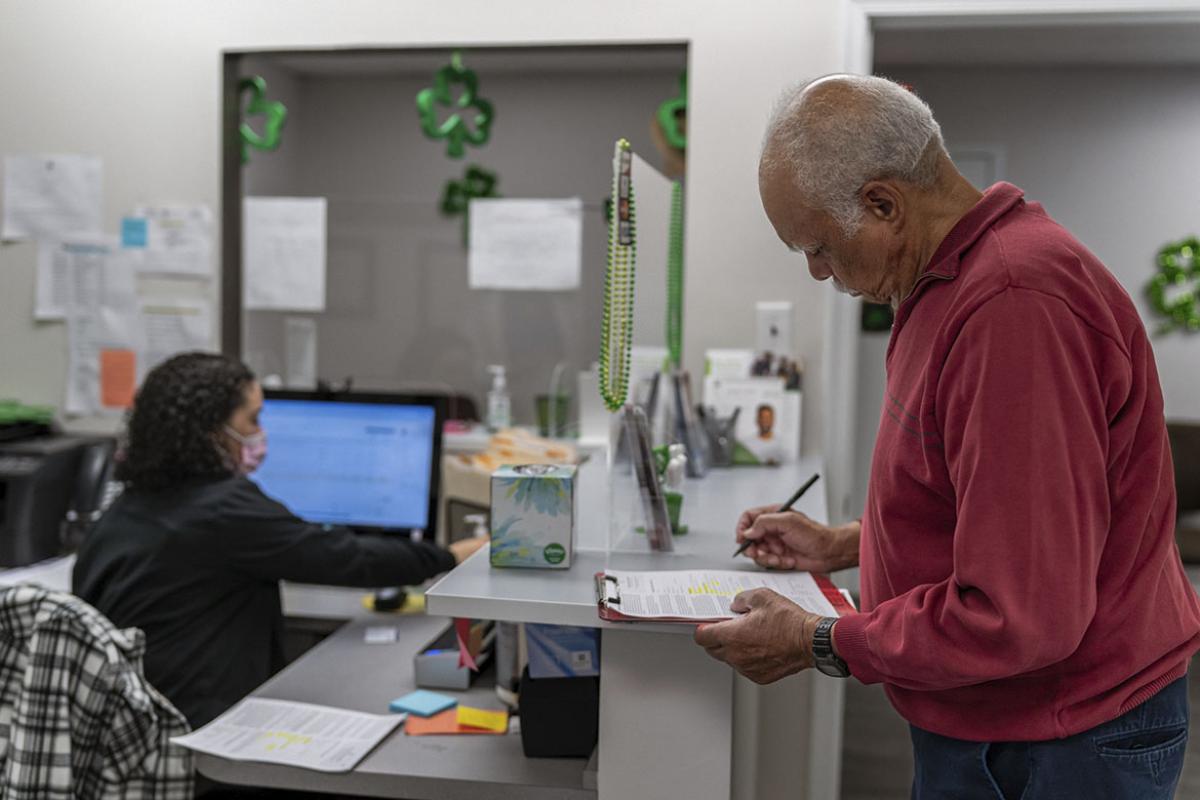
Physicians are finding that their patients can benefit when they formally refer them to a local program. This helps improve care continuity by establishing the program provider as a “practice extender” and as a member of the patient’s care team. It also helps ensure that patient data is circulating between the physician and the program’s operator, the presenters said.
The AMA assisted the YMCA of the USA on their CDC-funded demonstration project that worked with four local YMCAs and their partnering health care organizations in Seattle, Kansas City, New York City and Delaware. The YMCAs and health care partners attempted to implement bidirectional e-referral communication pathways and gain understanding of what EHR functions should be considered for these implementations.
Communication methods tested were: faxing information directly to EHRs, fully electronic communication between EHRs, and using clinical letters that contain key phrases to auto-fill patient-specific information in the EHR. The project involved 423 referrals between 2016 and 2018.
The heart of the matter
A key discovery of this IT project was that “the relationship is the centerpiece,” the presenters said.
“Health care providers shouldn’t let inadequate technology stop them from referring to community-based organizations,” Gakhar said. “Start low tech, figure out the best processes and workflow, then add the tech to support those processes once you’ve established the best approach.”
The presenters went so far as to say consider starting with paper referrals to streamline the process. It was also noted that an organization’s existing diabetes-management infrastructure can be leveraged to prevent type 2 diabetes.
Physicians can make these arrangements work for their practice, but it is recommended that they build a team that includes people in these key roles:
- Project lead—in charge of coordinating planning and implementation.
- Physician champion—engages with physicians to raise awareness and with leadership to gain organizational buy-in and supports care-team training.
- Population health coordinator.
- Health IT staffer.
- Marketing communications staffer—communicates with patients and works to reach new patients.
Trouble with interoperability
While patients are enrolled in the program, their physicians can be sent data to monitor their progress and then reinforce patients’ positive behavior change at their next clinical visits.
“Interoperability remains an enormous hurdle in moving information between health care providers and community-based organizations,” said Dr. Kirley, one of several AMA speakers at HIMSS this week. “It is imperative to overcome this barrier because patients need the services offered by community organizations to get healthy or stay healthy—they can’t rely entirely on the doctor’s office—but their doctor needs to stay in the loop to manage their care.”
The financial impact of this type of value-based care initiative was identified as a likely focus of future projects.