Contents
Preventive services can be provided at no cost to patients
Due to the Affordable Care Act (ACA), when physicians order certain evidence-based preventive services for patients, the insurance company may cover the cost of the service, with the patient having no cost-sharing responsibility (zero-dollar).
The ACA requires that most private insurance plans provide zero-dollar coverage for the preventive services recommended by four ACA designated organizations, specifically:
- U.S. Preventive Services Task Force (USPSTF)
- Advisory Committee on Immunization Practices (ACIP)
- Women’s Preventive Services Initiative
- Bright Futures
As coverage is directly aligned with these evidence-based recommendations, it is important to recognize which patient populations are eligible for each preventive service without cost-sharing and which patients may require cost-sharing for the same services and to ensure precise coding for qualifying preventive services.
How physicians and other health care providers help patients benefit
It is critical that physicians and other health care providers clearly communicate to payers through careful documentation and coding for health care items and services. Otherwise, insurance plans may not know that they are solely responsible for paying the patient’s bill, thus burdening the patient with a surprise bill for a fully covered preventive service.
Coding rules specific to ACA zero-dollar preventive services: Commercial payers
Confusion and inconsistency persist among payers, physicians, and other health care providers in coding and paying claims for preventive services. The AMA offers the following coding guidance to improve the billing process for all.
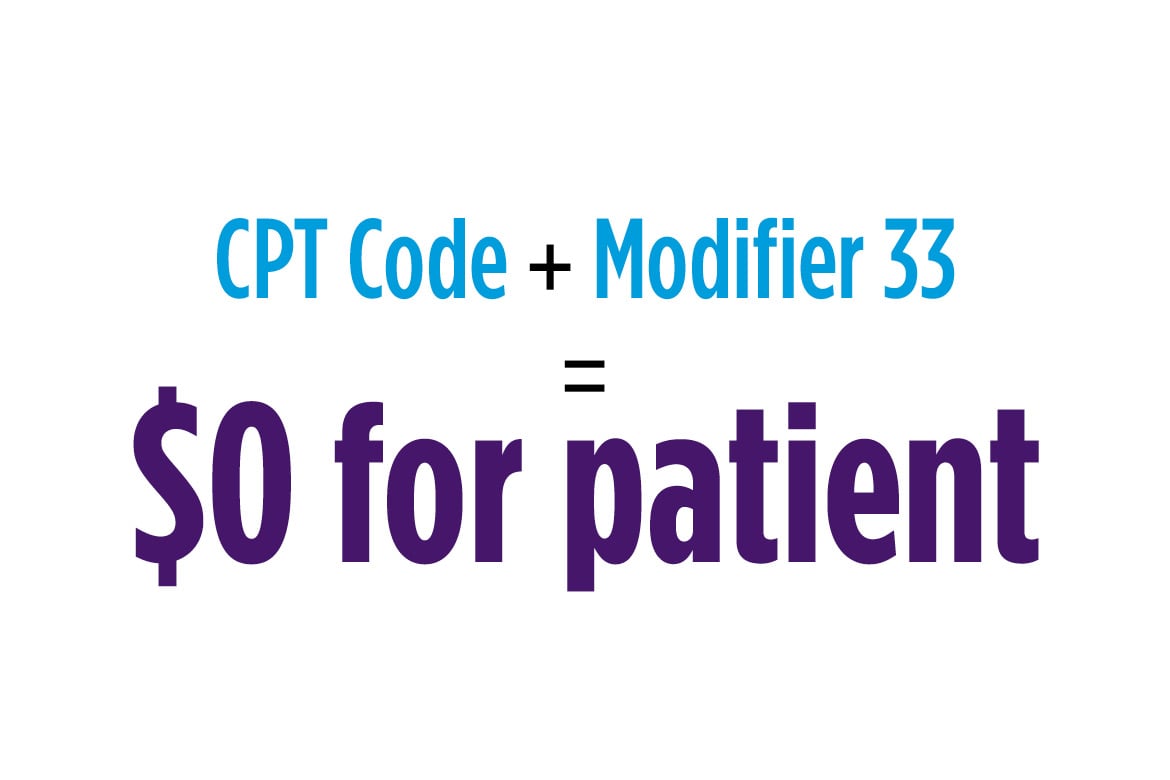
Current Procedural Terminology (CPT) modifier 33 can be used when billing for ACA-designated preventive services with a commercial payer. The addition of modifier 33 communicates to a commercial payer that a given service was provided as an ACA preventive service. The CPT modifier was developed to not only account for preventive services as defined under the ACA, it can also indicate unique circumstances (e.g., when a colonoscopy that was scheduled as a screening was converted into a diagnostic or therapeutic procedure).
Modifier 33 should be used when the primary purpose of the service is the delivery of an evidence-based service in accordance with the guidelines provided by one of the ACA-designated organizations, including an A or B recommendation from the USPSTF.
If physicians and other health care providers do not specify modifier 33, the insurance plan may think that the preventive service was for a patient who is not eligible for the zero-dollar benefit, and the patient may be billed. To be eligible for the zero-dollar benefit, patients must fall within the evidence-based recommendations provided by the by four ACA designated organizations.
To determine whether your patients qualify for zero-dollar preventive services:
Step 1
Consult one or more of the four ACA designated organizations for a current list of preventive services recommended, and thereby available with no patient cost-sharing for eligible patient populations. (Note: Services recommended by any one of these organizations must be covered without patient cost-sharing beginning one year following the date of recommendation).
- USPSTF Published Recommendations
- ACIP Recommendations
- Women’s Preventive Services Initiative Recommendations
- Bright Futures Recommendations
Step 2
Apply the appropriate CPT code(s) corresponding to the service rendered and be sure to also add modifier 33 to indicate that this is an ACA-designated preventive service.
Step 3
If you have any questions regarding correct CPT coding, the AMA’s CPT Network is available to AMA members and CPT Network subscribers.
Examples
Preventive service: Biennial screening mammography
Eligible for zero-dollar benefit: An average-risk woman 50 to 74 years of age*
Not eligible for zero-dollar benefit: Older or younger women, or women with certain breast cancer risk factors
*The USPSTF recommends screening starting at age 50, but Congress passed legislation to override the USPSTF to allow screening with no cost-sharing starting at age 40.
Preventive service: Colorectal cancer screening
Eligible for zero-dollar benefit: An average-risk, asymptomatic adult 50 to 75 years of age
Not eligible for zero-dollar benefit: Older or younger adults, or those with colorectal cancer symptoms or certain risk factors
Preventive service: Chlamydia and gonorrhea: Screening
Eligible for zero-dollar benefit: Sexually active women 24 years of age or younger and older women who are at increased risk for infection
Not eligible for zero-dollar benefit: Women older than 24 years of age who are not at increased risk for infection, and men
Preventive service: One-time screening for abdominal aortic aneurysm (AAA) with ultrasonography
Eligible for zero-dollar benefit: Men who are 65 to 75 years of age and who have ever smoked
Not eligible for zero-dollar benefit: Men who have never smoked, and all women
Coding rules specific to ACA zero-dollar preventive services: Medicare
Medicare was slow to adopt the CPT modifier 33 following its original publication in 2010. However, over time the modifier has received further guidance from Medicare Administrative Contractors (MACs). For instance, in 2015, Medicare announced that modifier 33 may be used when anesthesia is furnished in conjunction with a screening colonoscopy. In addition, in 2016, Medicare mandated the use of modifier 33 with Advance Care Planning services when provided on the same day as Annual Wellness Visits, so that any coinsurance and deductibles are waived.
Several preventive services covered by Medicare do not have a USPSTF recommendation grade of A or B. These include:
- Digital rectal examinations provided as prostate screening tests.
- Glaucoma screening.
- DSMT services.
- Barium enemas provided as colorectal cancer screening tests. (In the case of a screening barium enema, the deductible is waived under another section of the statute.)
In these scenarios, modifier 33 is not applicable.
The Medicare program has established modifier PT, which denotes when a service began as a colorectal cancer screening test and then was moved to a diagnostic test due to findings during the screening. In this instance, the modifier PT is appended to the diagnostic procedure code that is reported instead of the screening colonoscopy or screening sigmoidoscopy HCPCS code.
In general, practices should consult local MACs to determine the appropriate rules for reporting preventive services within the Medicare program and visit the Medicare Preventive Services website for more details.
Preventive care and COVID-19
AMA talks to health experts about the importance of preventive care and how physicians help their patients access certain preventive services at no cost to the patient.
Information provided by the AMA does not constitute clinical advice, does not dictate payer reimbursement policy, and does not substitute for the professional judgment of the practitioner performing a procedure, who remains responsible for correct coding.
Table of Contents
- Preventive services can be provided at no cost to patients
- How physicians and other health care providers help patients benefit
- Coding rules specific to ACA zero-dollar preventive services: Commercial payers
- Coding rules specific to ACA zero-dollar preventive services: Medicare
- Preventive care and COVID-19