The rapid appearance of the COVID-19 pandemic in the United States forced many physician practices into what—for them—was the unchartered world of telemedicine. Telehealth was a viable solution for many practices because it allowed them to leverage key technological tools to continue seeing patients, be it for a COVID-19 diagnosis or for a separate chronic condition.
For The Permanente Medical Group (TPMG)—an AMA Health System Program Partner—though, telemedicine is a technology that has been in place for more than 20 years. One aspect of the group’s overall telehealth offerings is its teledermatology program, which has been in place in Northern California for nearly 15 years.
While TPMG has adjusted to the rise of the coronavirus, the success of its teledermatology program provided useful guidance in how to care for patients who could not—or would not—leave their homes during stay-at-home orders.
“Teledermatology has taught us the value of driving performance with technology,” said Richard S. Isaacs, MD. He is CEO and executive director of TPMG, president and CEO of the Mid-Atlantic Permanente Medical Group, and co-CEO of the Permanente Federation. “We have dramatically ramped up our telehealth strategy and are maximizing our technology and integration in ways we haven’t done before.”
About 80% of the outpatient care systemwide is now provided through video and telephone visits, Dr. Isaacs said. In Northern California, TPMG is performing nearly as many video visits on average in one week than it conducted in all of 2019 . Additionally, almost 60% of prescriptions are being filled through the system’s mail-order pharmacy operations, compared with 32% prior to the pandemic.
Patients are given the option of how they want to connect with their doctor or other clinician—by video, phone, secure messaging, or in-person visit. However, the emphasis on telehealth has allowed TPMG to substantially reduce the number of patients entering its medical centers and offices and help mitigate the spread of the novel coronavirus.
Patient satisfaction, meanwhile, has not suffered.
“This approach has clearly driven patient convenience and effective care without delay across our program,” Dr. Isaacs said. “And many of our patients who have not previously used our telehealth services have told us that they greatly appreciate the ease, convenience, and value of telehealth.”
The rise of teledermatology
There has been a national shortage of dermatologists for decades. A 2016 article in JAMA reported that in the United States, there are fewer than 3.4 dermatologists for every 100,000 people.
Meanwhile, the U.S. population continues to grow older. The U.S. Census Bureau predicts that by 2030, one in every five Americans will be 65 or older and that by 2060, there will be more than 94 million Americans who are 65 or older, nearly twice as many as there are today.
“There’s an aging population, and there’s a lot of skin out there,” said Dr. Isaacs. “One in five people in the country develop skin cancer, but there is a plethora of benign skin conditions that also require the expertise of the dermatologist. So, you have increasing demand and a limited supply of dermatologists.”
It was that imbalance in supply and demand that led TMPG to launch a teledermatology program that is now one of the largest in the country, with more than 170,000 virtual interactions between dermatologists and patients in 2019. TPMG hosted more than 200,000 teledermatology video visits, and in early 2020, prior to the COVID-19 pandemic, 70% of dermatology visits in the system’s Northern California locations were conducted using telehealth. In the past two months, during the pandemic, more than 95% of TPMG’s dermatology visits have been virtual.
Learn more about five disruptive trends transforming health care.
How the teledermatology program works
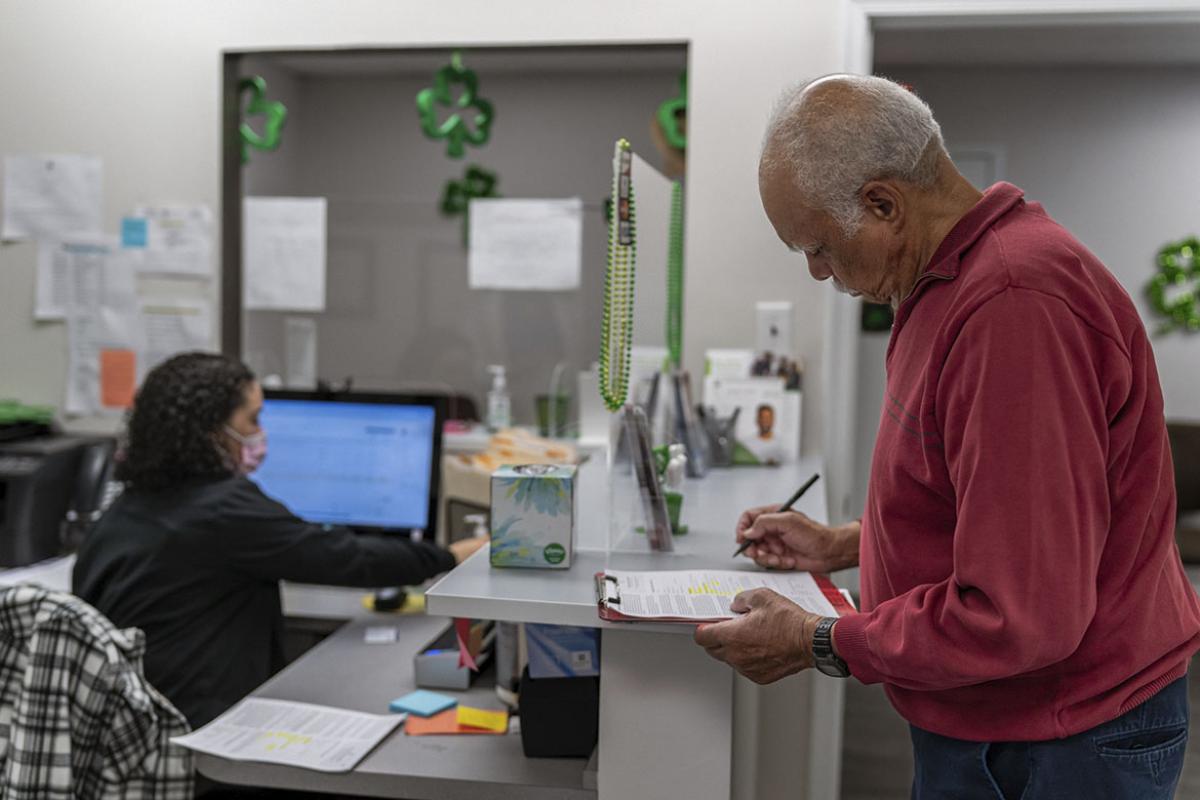
A basic example of how the TPMG teledermatology program works involves a patient who is concerned about a suspicious lesion or mole on their body. The patient can take a picture of the location in question and send it to their primary care physician for review. The physician can request the patient come in for a more thorough evaluation, or if the physician determines that a dermatologist should be involved, they can send the photo to an on-call dermatologist to review.
If the patient does an in-person evaluation, the physician can also take a higher-quality image and forward that to a dermatologist. The dermatologist can then decide whether there is a problem, if a prescription is needed, or if there should be an in-person evaluation and potential biopsy.
A study in the Journal of the American Academy of Dermatology in 2019 found that when TPMG dermatologists had the chance to look at well-photographed skin lesions, they were able to identify nearly 10% more cancers with almost 40% fewer referrals to the dermatology department.
Dr. Isaacs said that even though patients who use the teledermatology program are remote, they still benefit from a personal connection with their dermatologist.
“There is a personal touch, it’s just [through] a different vehicle,” he said. “It’s a personalized experience. It’s essentially a conversation with the physician, so it’s just as personal.”
Learn how the AMA’s digital health leadership ensures physicians are represented in the development of new health care technologies.
Medicine’s future got here faster
Dr. Isaacs is not shy about his vision for what health care will look like in the coming years.
“We think [telehealth] is the future of healthcare delivery in this country,” he said. “If you need to connect to care, you should be able to have a virtual, on-demand session when and where you need it.”
TPMG has routinely shared its experience with teledermatology and other telehealth programs with the larger medical community in order to help others better understand how it is organized and how it can make the healthcare system more effective, affordable, and accessible.
“What we’ve learned from our telehealth program overall during the current COVID-19 pandemic is that the patients love this way of interacting with our physicians and clinicians because it provides timely access to care and the convenience of speaking with a physician from their own home,” Dr. Isaacs said. “Telehealth demonstrates our patient-centered approach to care and our commitment to delivering high-quality care to our members and patients where and when they need it, and that doesn’t have to be an in-person visit.”
Amid the ceaseless tragedy of the COVID-19 pandemic there’s a small silver lining in the accelerated adoption of telemedicine, said Dr. Isaacs.
“We’re moving health care in the direction that we were trying to go,” he said, “but we’re going there faster.”