Primary care practices see patients with untreated and undertreated mental illness every day, although many feel they cannot adequately address their patients’ behavioral health needs. Meanwhile, many patients would prefer to access mental health treatment at their primary care visits, with the physicians who know them best. Two organizations have successfully piloted integrated behavioral health services and share their insights on the benefits and obstacles encountered.
A ReachMD podcast episode, “Behavioral Health Integration: Exploring Its Effect on Clinical Practice,” sponsored by the AMA, explains the benefits and challenges of integrated behavioral health services experienced by these two practices.
“Twenty percent of the population will at some time have a mood disorder, 29% will have an anxiety disorder, 17% or greater will have a substance-use disorder, and 2% have psychosis,” said Donald Meyer, MD, in the podcast, which is part of the “Reaching the Potential of Value-Based Care” series.
Dr. Meyer is assistant professor of psychiatry at Harvard Medical School and staff psychiatrist with the Mount Auburn Cambridge Independent Practice Association. He added that physicians are also tasked with managing populations.
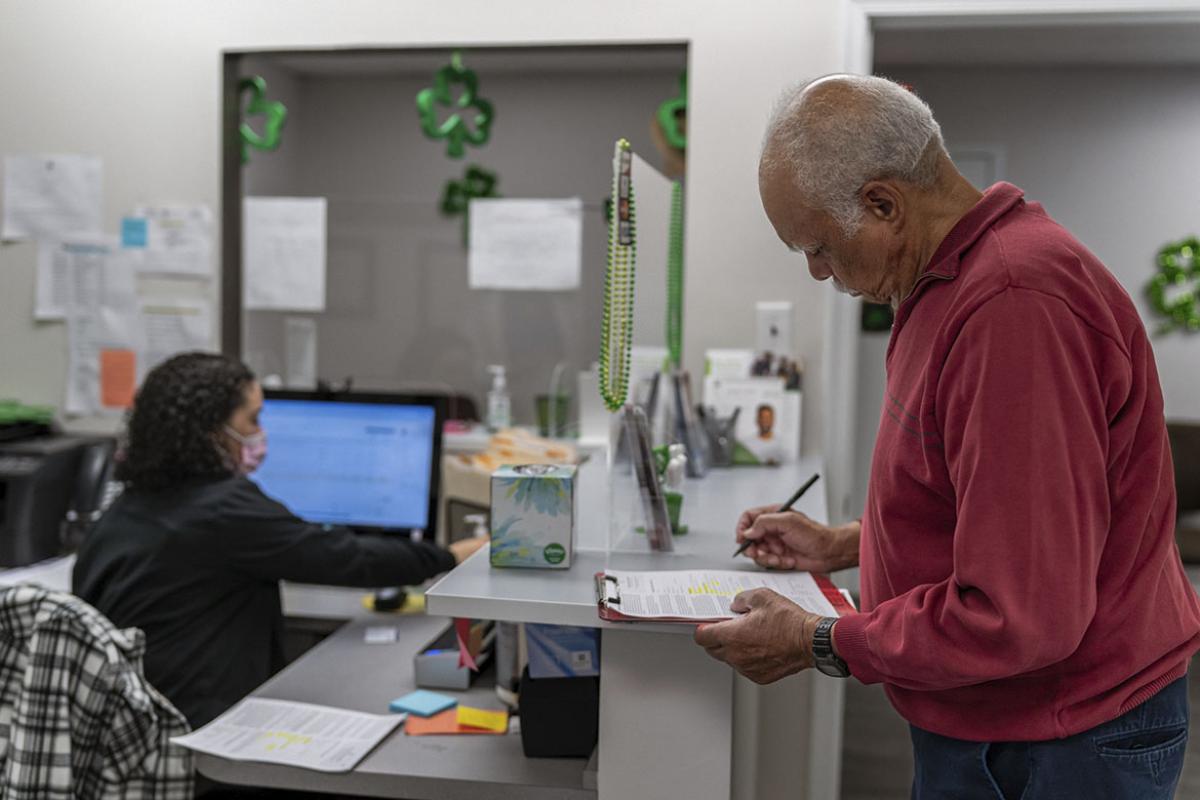
Meanwhile, many patients have said they would feel more comfortable having mental health concerns addressed within their primary care visits to avoid the stigma and added step of making an appointment with a specialist.
But primary care physicians are not always well trained in managing mental health issues, “so it was quite clear that the only way to address that concern would be to integrate mental health professionals into primary care,” said Travis Mickelson, MD, medical director of mental health integration at Intermountain Healthcare in Utah.
Massachusetts, Utah examples
With the help of a grant to study cost savings and health care outcomes using a collaborative care model, Mount Auburn Cambridge adopted a two-pronged goal: to identify where these two groups overlap and create avenues of intervention. With its primary care physicians grouped into pods, they identified a metabolic specialist in each pod.
“We hired health care coaches who were post-bachelor degree individuals interested in medicine and psychology and trained them in motivational interviewing, in formulating small steps a patient could take to improve their health,” Dr. Meyer said. “And we had psychiatrists deployed to each of the pods to meet with metabolic specialists and a pods health care coach to share information and make plans.”
Intermountain’s integrated behavioral health program was started by an advanced practice registered nurse and a couple of pediatricians.
Part of what the two programs had in common was “having someone on that team, within that primary care clinic, that plays the role of the health advocate or care manager,” Dr. Mickelson said. “Because one of the important aspects of any successful behavioral health or mental health integration model is we need some added support to help that primary care provider and the psychiatrist. This is not something that only a psychiatrist or primary care provider is going to be able to adequately manage on [their] own.”
All about improved outcomes
“One of the most satisfying things about these programs is that we saw the hoped-for differences,” Dr. Meyer said of Mount Auburn Cambridge’s efforts. “So if you look at the aggregate scores on PHQ-9s, they improved dramatically because of these programs. And if you look at hemoglobin A1cs or blood-pressure control, those improved as well.”
One of the biggest challenges in developing behavioral health integration programs, Intermountain’s Dr. Mickelson added, is changing organizational culture.
“It's important for us to be able to show them [primary care physicians] why this work matters,” he said. “We can actually decrease the primary care stress and burden that they're under. And also, if we can do this in a way that really measures outcomes, we can show that we are improving quality and decreasing the high cost of care.”