For physicians to be at their best, it is important to achieve a balance between their personal and professional lives. In an effort to support physicians’ passion for the practice of medicine, a Minnesota health system looked to cut down on the so-called pajama time that doctors spend on after-hours administrative work.
By asking physicians to complete a survey, HealthPartners, an integrated, nonprofit health care organization in Bloomington, Minnesota, identified areas for improvement. One area of opportunity focused on time spent working, which included administrative work done outside of the time physicians spend directly with patients. This correlated highly with the group’s overall satisfaction.
“It would be great if decreasing time spent working only required a single work plan or initiative,” HealthPartners Chief Operating Officer Nance McClure said in an AMA STEPS Forward™ module. “However, we learned our approach must include multiple initiatives working towards the same goal."
HealthPartners pursued these three strategies that saved physicians more than 30 minutes a day.
Define a standard set of workflows and create stable teams. HealthPartners defined workflows focused on creating procedures and protocols for care teams to provide a consistent clinical experience for patients. Through standardized workflows and stable care teams, physicians save about 30 minutes per day.
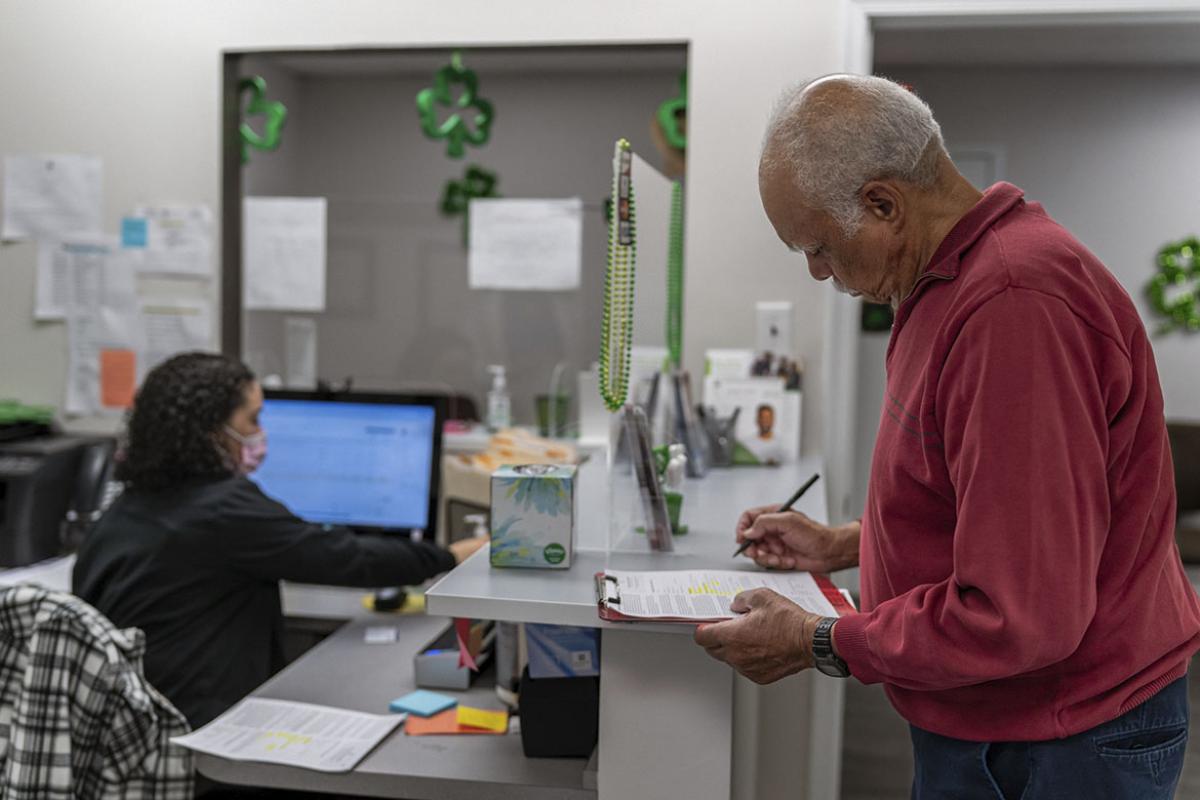
The core care team typically includes a physician, nurse and receptionist. Some clinics might also have a pharmacist or dietitian on the team, while larger practices may include a behavioral-health therapist. The goal is to make the best use of collective skills.
Teams plan for patient interactions in defined cycles that include scheduling, pre-visit planning, check-in, visit and post-visit. This allows teams to anticipate patient needs and provide follow-up care. For example, pre-visit planning might include identification of preventive care services and contacting the patient to schedule lab tests before their appointment. If planning is not completed prior to a patient’s visit, it will be completed during the rooming process.
Standardized workflows and stable care teams also allow for easy transitions between staff due to turnover, sick days or vacations.
Improve documentation for consistency and clarity. Physicians save a total of 30 minutes a day through streamlined electronic health record documentation. Some of the improvements that have been made to enhance documentation include:
- Careful use of best-practice alerts.
- Availability of more than 40 templates for collaborative documentation between nurses and physicians.
- Co-located workspaces to support social interactions.
- Wider monitor screens.
- Printers in exam rooms.
Shared nurses work with three-to-four physicians at a time and use a designated EHR template to free up the doctor’s time. In a shared visit for patients with complex medical needs, the nurse also covers medication reconciliation and history of illness during the rooming process to leave more time for the physician to spend with the patient.
Ongoing work to efficiently manage in-baskets. To help physicians save 15 minutes a day, “blinded” in-baskets—visible to only one user—were eliminated. This allowed for work to be redistributed across the entire care team instead of resting solely with physicians.
For example, due to consistent training and availability of educational resources, the rooming staff prioritizes messages for review and handles nonemergent messages. The goal is to have other care team members maintain as many messages as possible so the physician can spend more one-on-one time with the patient.
Streamlined test results also freed up the in-basket. About 95 percent of lab test results are automatically released to patients through the patient portal, which provides quicker results and frees up phone lines.
AMA’s STEPS Forward is an open-access platform featuring more than 50 modules that offer actionable, expert-driven strategies and insights supported by practical resources and tools. Based on best practices from the field, STEPS Forward modules empower practices to identify areas or opportunities for improvement, set meaningful and achievable goals, and implement transformative changes designed to increase operational efficiencies, elevate clinical team engagement, and improve patient care.
Several modules have been developed from the generous grant funding of the federal Transforming Clinical Practices Initiative (TCPI), an effort designed to help clinicians achieve large-scale health transformation through TCPI’s Practice Transformation Networks.
The AMA, in collaboration with TCPI, is providing technical assistance and peer-level support by way of STEPS Forward resources to enrolled practices. The AMA is also engaging the national physician community in health care transformation through network projects, change packages, success stories and training modules.